In part one, we discussed important terms and concepts about the conduction system of the heart and fundamental components of an ECG strip. In part two, we reviewed analyzing and measuring the different components of a ECG rhythm strip. In part three of this series, we will discuss how to identify the main heart rhythms and appropriate interventions that new grads will need to be able to answer NCLEX style questions pertaining to ECG interpretation.
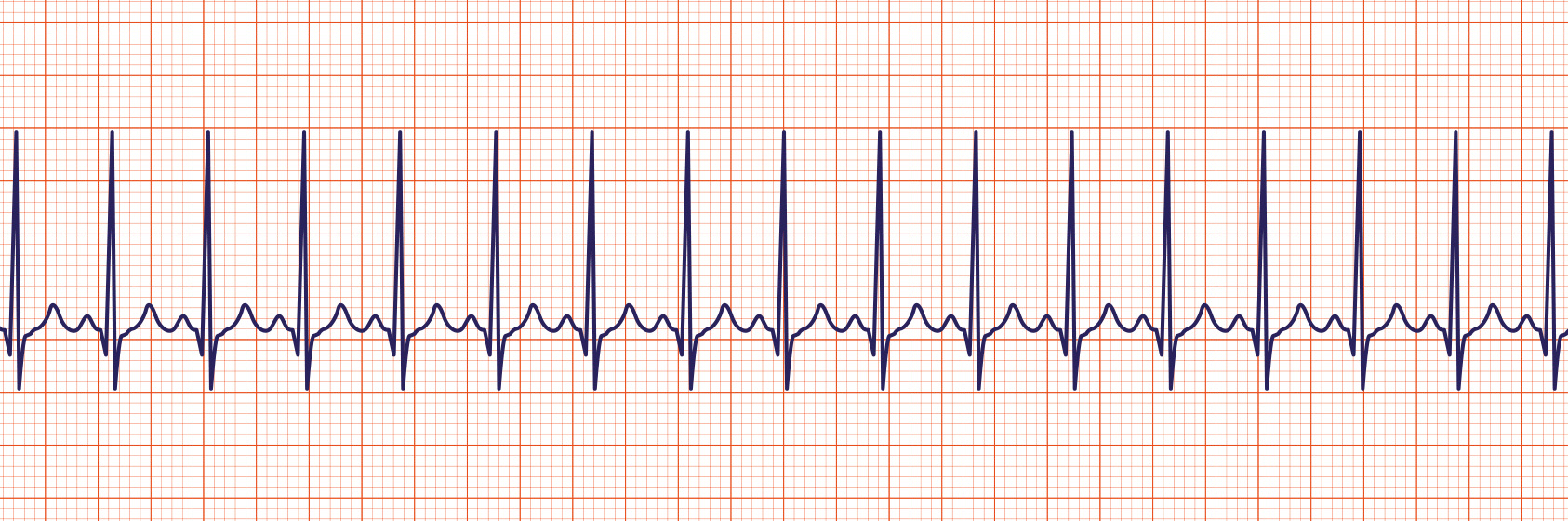
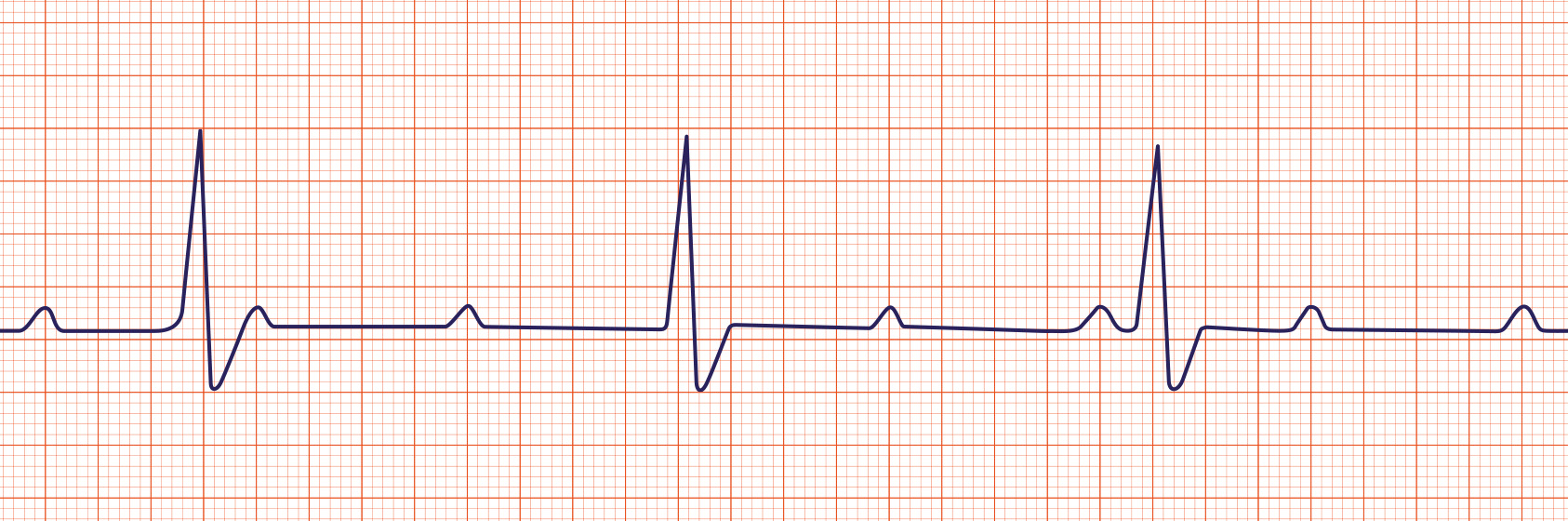
Identifying Normal Sinus Rhythm
Normal Sinus Rhythm is a regular or expected heart rhythm for a healthy adult. The rhythm will have normal P, Q-R-S, T deflections and intervals. The heart rate will be between 60-100 at rest.
Normal Sinus Rhythm Interventions: Document the Normal Findings, and Continue to Monitor the Patient.
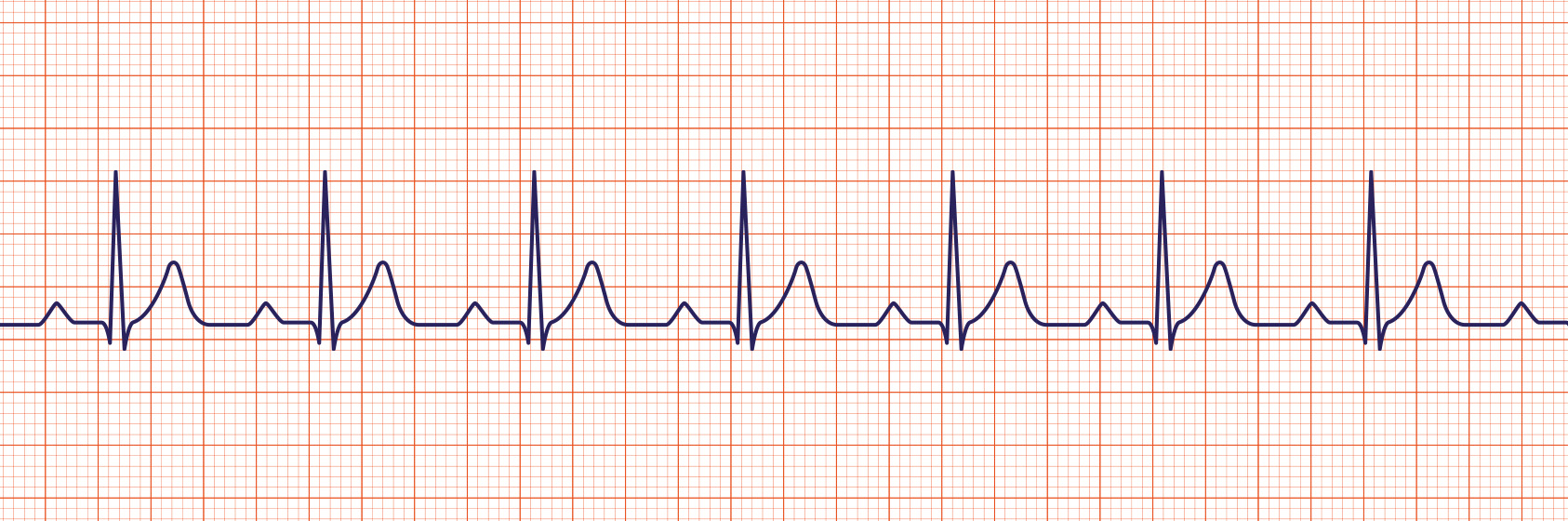
Identifying Sinus Bradycardia
Sinus Bradycardia is a sinus rhythm with a rate of less than 60 per minute in an adult. The rhythm will have normal P, Q-R-S, T deflections and intervals. Sometimes athletic individuals could have a resting heart rate of less than 60 beats per minute. Sinus bradycardia only becomes an issue if the patient becomes symptomatic.
Asymptomatic Sinus Bradycardia Interventions: Assess for Cause, Document, Notify the Provider, and Continue to Monitor.
Symptomatic Sinus Bradycardia Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath, Signs of Decreased Cardiac Output): Call Rapid Response, Prepare for Transcutaneous Pacing, Give Atropine.
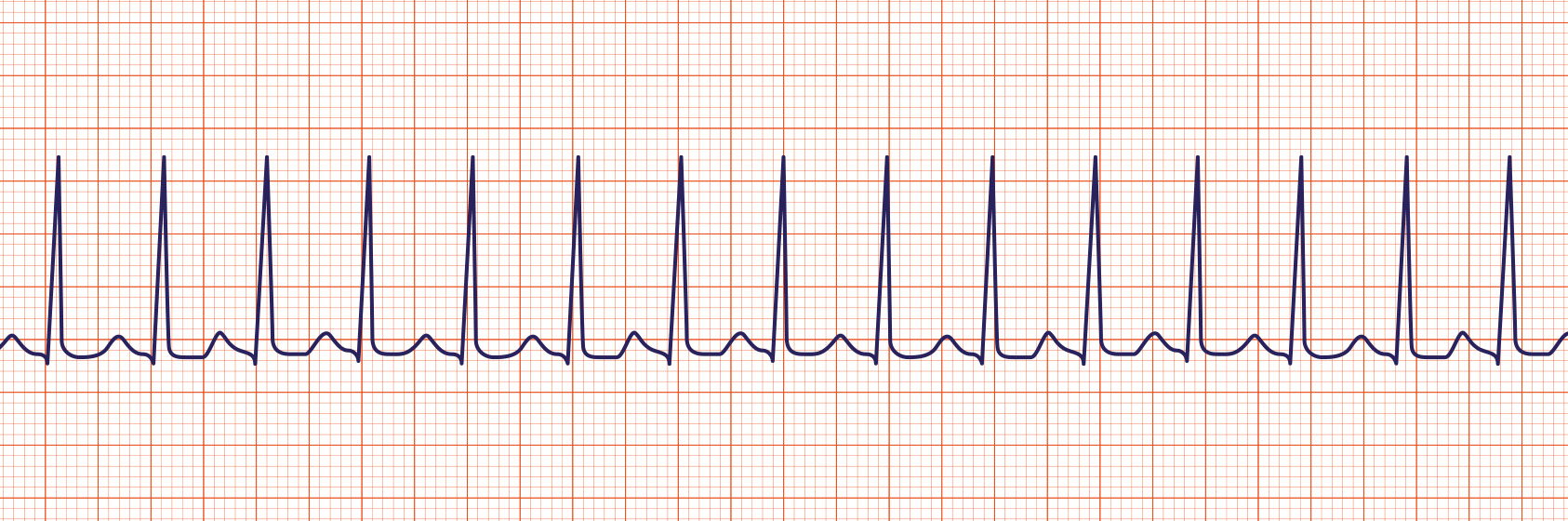
Identifying Sinus Tachycardia
Sinus Tachycardia is a sinus rhythm with a rate greater than 100 per minute in an adult. Note that the p waves are still present. The rhythm will have normal P, Q-R-S, T deflections and intervals. Sinus Tachycardia can be caused by a variety of factors such as Pain, Fever, Dehydration, Fear, Anger, Anxiety, Caffeine, Medications, and other underlying conditions. If Sinus Tachycardia is sustained, it can become a problem for a patient, so we must act so we can get the heart rate closer to a normal rate.
Asymptomatic Sinus Tachycardia Interventions: Assess for Cause, Document, Notify the Provider, and Continue to Monitor.
Symptomatic Sinus Tachycardia Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Cardioversion, Give Adenosine.
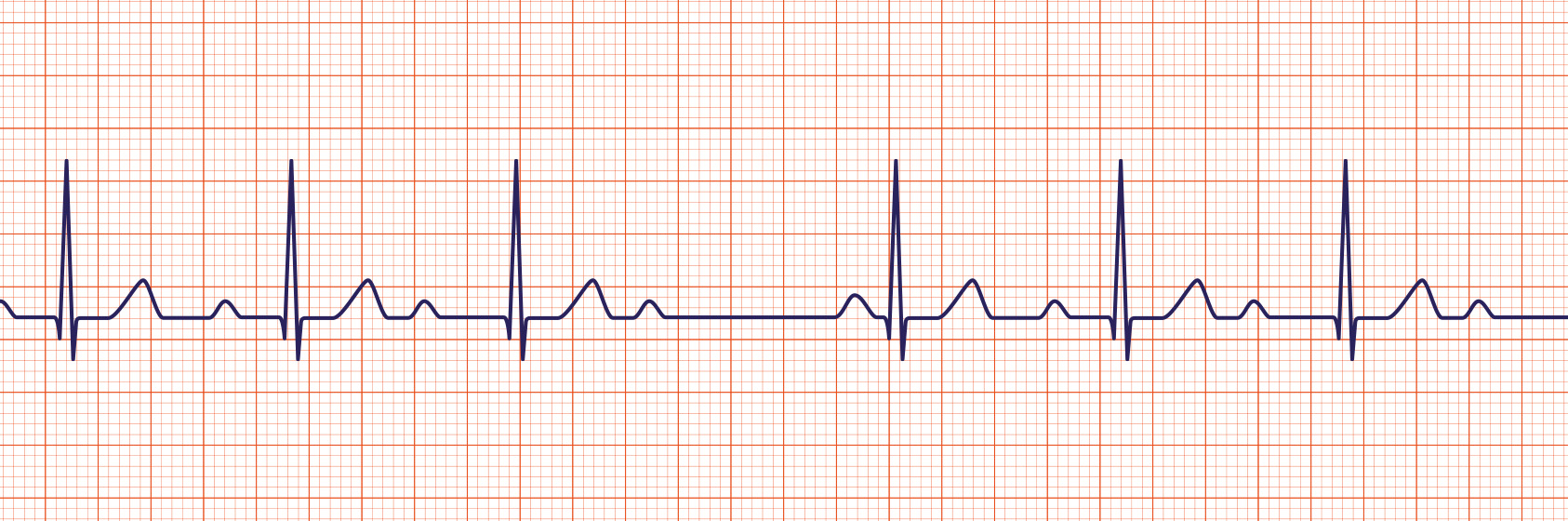
Identifying First-Degree Heart Block
1st degree heart block is a sinus rhythm with a prolonged PR interval > 0.20 seconds, which is caused by a delay in electrical conduction from the SA node in the atria, to the AV node in the ventricles. There are many reasons why this can happen, but the common reasons include medications, and heart disease or damage to the heart. The essential thing to consider is that the longer the PR interval becomes, the slower the heart rate will be. First Degree Heart Block only becomes an issue when the patient is symptomatic.
Asymptomatic 1st Degree Heart Block Interventions: Assess for Cause, Notify the Provider, Document and Continue to Monitor.
Symptomatic 1st Degree Heart Block Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Transcutaneous Pacing, Give Atropine (if bradycardia is present).
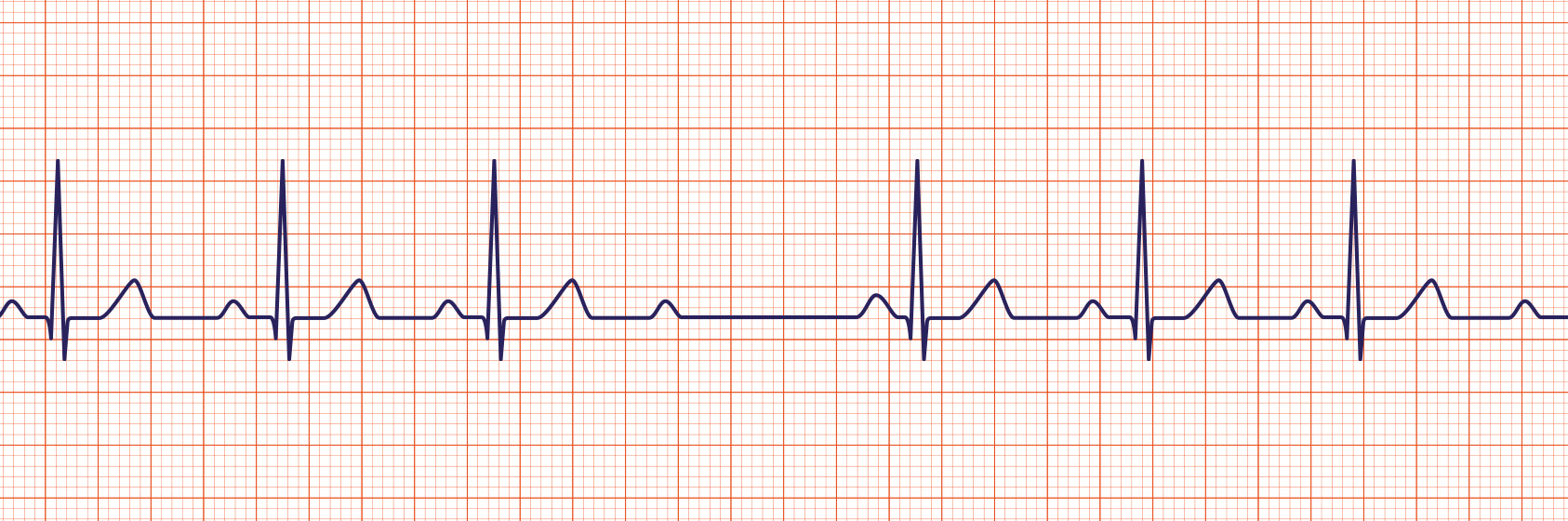
Identifying Second-Degree Heart Block Types I & II
A 2nd degree heart block is usually classified as either Mobitz Type I (AKA Wenckebach) or Mobitz Type II.
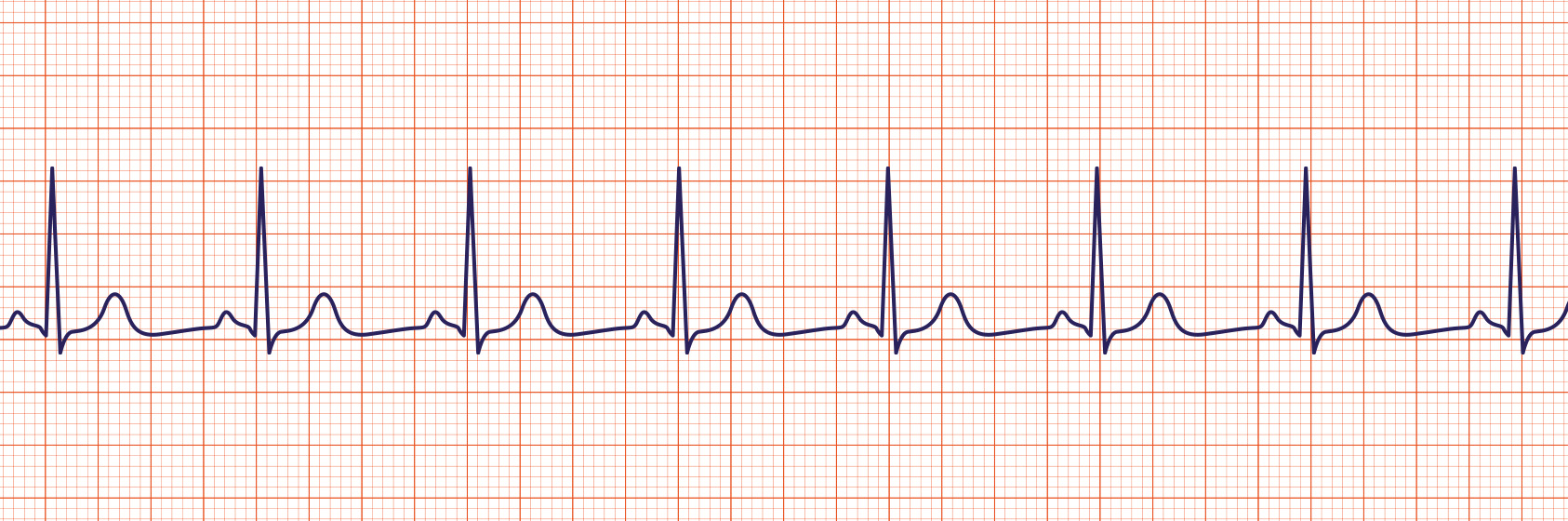
A Mobitz Type I heart block is characterized by progressive lengthening of the PR interval until a QRS complex is dropped. You can see in the strip below that the PR intervals get longer with each complex, until conduction is completely lost, thus the electrical signal that normally stimulates the ventricles of the heart to contract does not fire, and a heart beat is skipped.
“Long, Long, Longer – DROP! Now, you’ve got a Wenckebach!“
Second Degree Heart Block Type I (Mobitz I or Wenckebach) only becomes a problem is the patient is symptomatic.
Asymptomatic 2nd Degree Heart Block Interventions: Assess for Cause, Notify the Provider, Document and Continue to Monitor.
Symptomatic 2nd Degree Heart Block Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Transcutaneous Pacing, Give Atropine (if bradycardia is present).
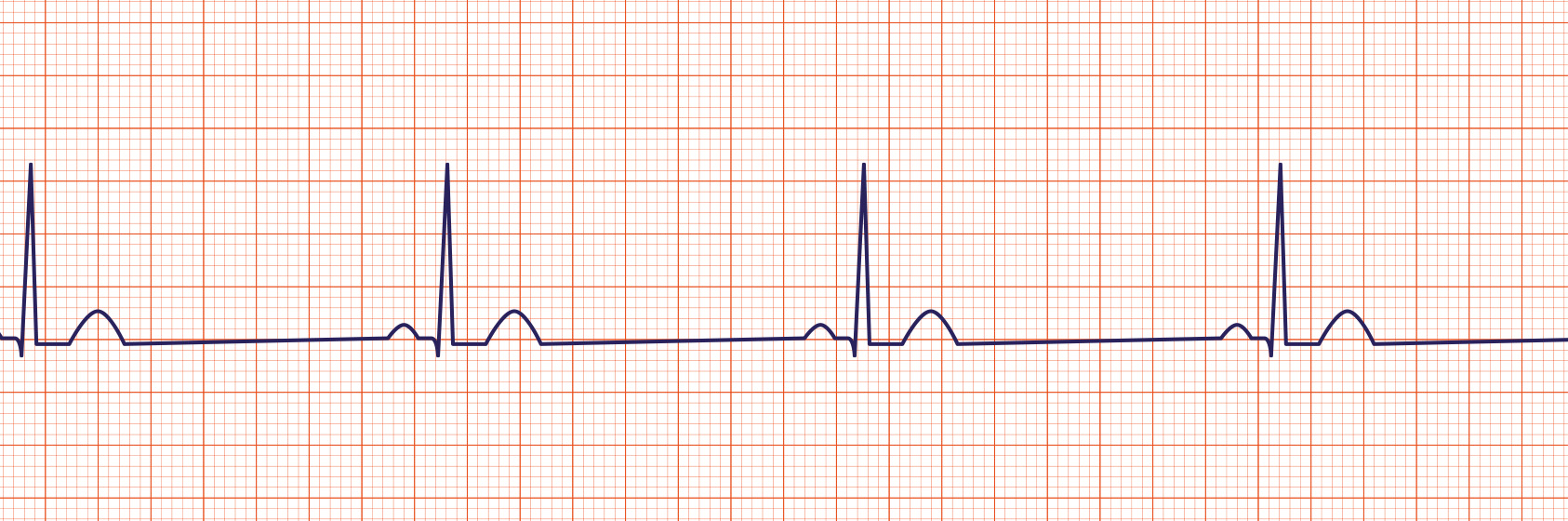
A Mobitz Type II heart block is characterized by an intermittent dropped QRS that is not in a Mobitz Type I pattern. The Mobitz Type II block must be evaluated since it is one that can rapidly progress to a complete heart block.
Second Degree Heart Block Type II (Mobitz II) only becomes a problem is the patient is symptomatic.
Asymptomatic 2nd Degree Heart Block Interventions: Assess for Cause, Notify the Provider, Document and Continue to Monitor.
Symptomatic 2nd Degree Heart Block Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Transcutaneous Pacing, Give Atropine (if bradycardia is present).
Identifying Third-Degree Heart Block
A 3rd degree heart block (sometimes called a complete heart block) is a rhythm in which there is no relationship between the P and QRS waves. In this case, the P waves have no relationship to the QRS complexes on the ECG. This rhythm is dangerous because it is associated with bradycardia that cannot sustain adequate perfusion. If you see this rhythm, always assess your patient right away!
Asymptomatic 3rd Degree Heart Block Interventions: Assess your patient right away, Assess for Cause, Notify the Provider Immediately, Document and Continue to Monitor.
Symptomatic 3rd Degree Heart Block Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Transcutaneous Pacing, Give Atropine (if bradycardia is present).
Identifying Supraventricular Tachycardia
Supraventricular tachycardia (SVT) is an extremely fast atrial rhythm with narrow QRS complexes. The name comes from the fact that the electrical impulse originates above the bundle branches (above the ventricles).
Just remember the Song from Mary Poppins – “SUPRA-califragilisticexpialidocious” – it’s fast, upbeat, and could easily wear one out! If sustained, Supraventricular Tachycardia can cause the patient to become symptomatic, so we must act fast to get the patient’s heart rate closer to normal.
Asymptomatic Supraventricular Tachycardia Interventions: Assess for Cause, Document, Notify the Provider Immediately, and Continue to Monitor.
Symptomatic Supraventricular Tachycardia Interventions (Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Cardioversion, Give Adenosine.
Identifying Atrial Fibrillation
Atrial Fibrillation ( AKA Afib or AF) is a very common atrial arrhythmia. This rhythm is characterized by no identifiable P waves before each QRS complex and the intervals between each QRS complex are irregular. This rhythm means the atria of the heart are quivering and not fully contracting. The electrical impulse from the SA node is not conducting properly, and the results are a short-circuit-like response.
A-fib in itself is not really a problem. Most patients don’t even feel when they are in atrial fibrillation. The problem lies in the fact that the blood does not fully eject out of the atria with each heartbeat because the atria are not fully contracting.
As that blood swishes around, it starts to clump together, which causes these patients to develop blood clots. These blood clots can travel to different parts of the body and cause major issues like Pulmonary Embolisms, Deep Vein Thrombosis, Heart Attacks and Stroke.
Additionally, patients with A-fib are at risk for entering into a dangerous tachycardia (Called A-fib with Rapid Ventricular Response), which would be treated similarly to SVT. Sometimes these patients will be scheduled for a procedure called an ablation, where the part of the heart that is causing the a-fib will be zapped, so that the cells responsible for the irregular rhythm are killed, and so the SA node can take over and cause the atria to contract at a regular rate.
Asymptomatic Atrial Fibrillation Interventions: Assess cause, Notify the Provider Immediately, Check to see if patient is on anticoagulants, Document and Monitor.
Symptomatic Atrial Fibrillation Interventions (Tachycardia, Palpitations, Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Cardioversion, Give Calcium Channel Blocker or Beta Blocker.
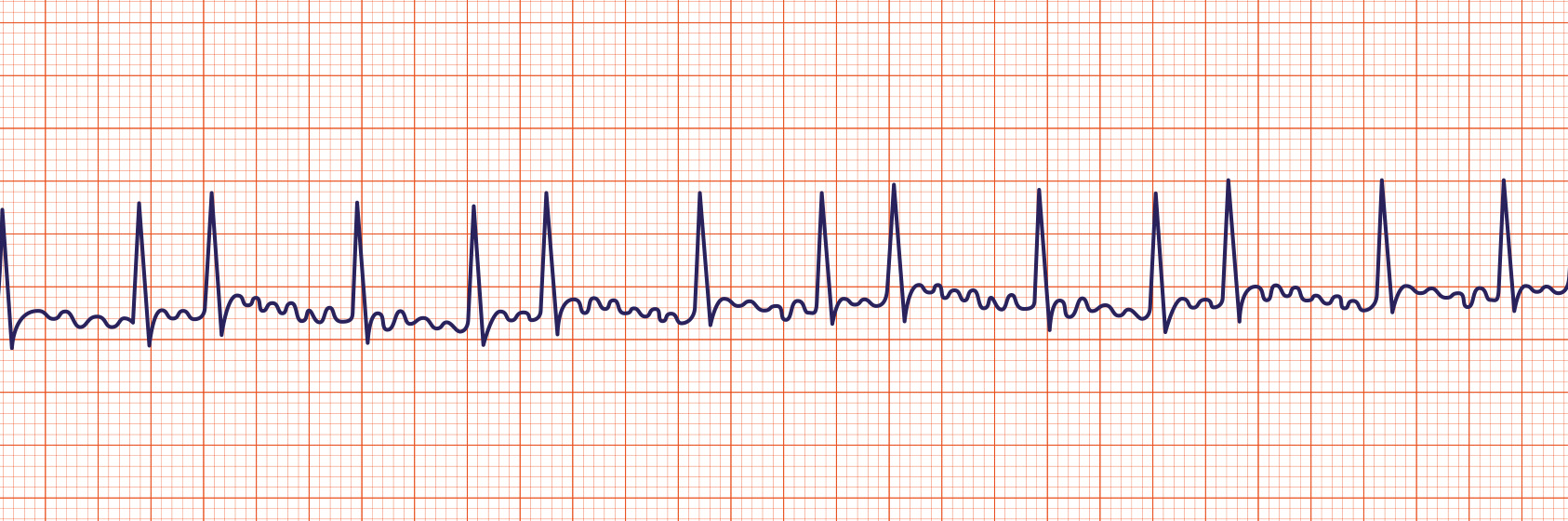
Identifying Atrial Flutter
Atrial flutter is a supraventricular arrhythmia (atrial arrhythmia) that is characterized by a “saw-toothed” flutter appearance on the ECG that represents multiple P waves for each QRS complex. A flutter can have a regular or irregular interval between each QRS complex. The key identifying factor is that there are MULTIPLE P Waves in between each QRS complex.
Atrial flutter in itself is not really a problem for patients. In most cases, a-flutter does not cause any issues with adequate perfusion. It only becomes a problem if it coverts over to a-fib, or if the heart rate becomes too elevated. If the rhythm coverts over to a-fib, we need to make sure the patient is being covered with anticoagulants to prevent blood clots. Sometimes, these patients will be scheduled for a procedure called an ablation, where the part of the heart that is causing the a-flutter will be zapped, so that the cells responsible for the irregular rhythm are killed, and so the SA node can take over and cause the atria to contract at a regular rate.
Asymptomatic Atrial Flutter Interventions: Assess cause, Notify the Provider Immediately, Document and Monitor.
Symptomatic Atrial Flutter Interventions (Tachycardia, Palpitations, Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare for Cardioversion, Give Calcium Channel Blocker or Beta Blocker.
Identifying Asystole
Asystole is also commonly known as a “flat line” where there is no electrical activity seen on the cardiac monitor. Unlike what you may see on TV – this rhythm is NOT responsive to electrical defibrillation. We do NOT shock when someone flatlines! This is not an episode of Scrubs!
Asystole Interventions: Assess Patient and Check for Pulse and/or Breathing. If no pulse or breathing, Call a Code! If the patient is a Full Code, Begin delivering High-Quality CPR. Attach the Patient to the AED in the event that they covert into a shockable rhythm. Follow ACLS Protocol to resuscitate the patient.

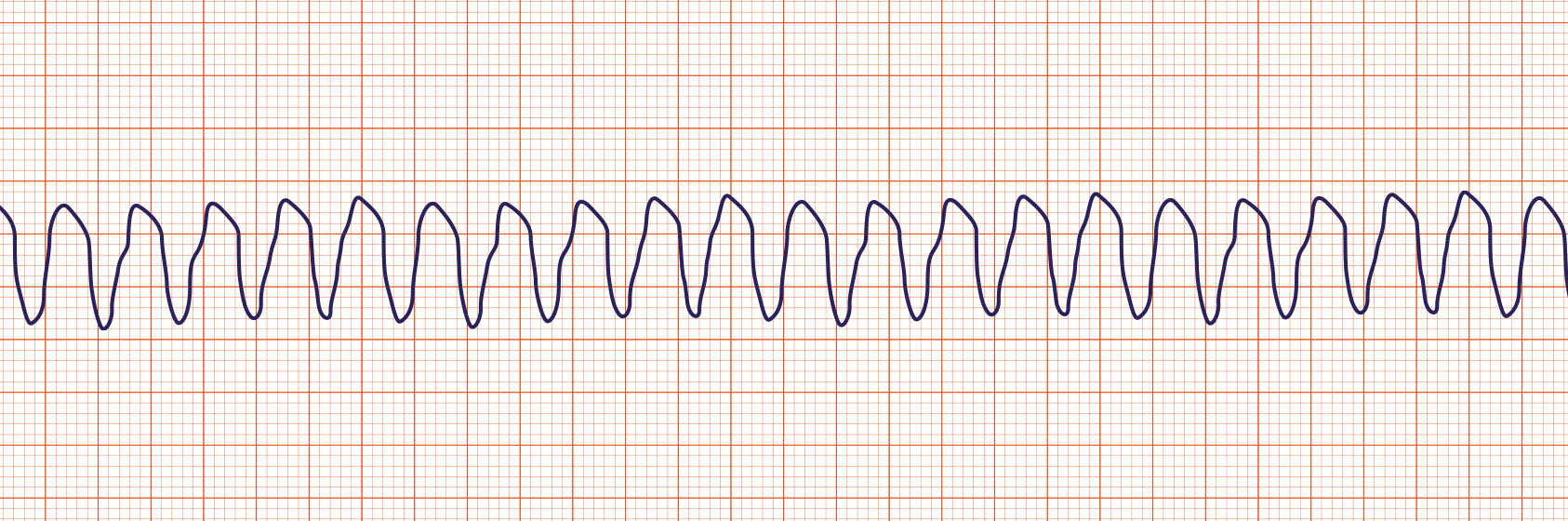
Identifying Ventricular Tachycardia
Ventricular tachycardia (Vtach or VT) is a ECG Rhythm that is characterized by bizarre widened QRS complexes, no P waves and usually a rate over 100 per minute. Vtach may quickly covert to Ventricular Fibrillation, and even death. Vtach is one of the two “Shockable Rhythms”, which means it may be responsive to electrical defibrillation.
When a you see Vtach on the monitor, it is essential that you immediately assess your patient to determine if they are asymptomatic or symptomatic.
Asymptomatic Ventricular Tachycardia Interventions: Immediately Assess your Patient, If alert and able to follow instructions, have your patient cough forcefully, or bear down like they are trying to have a bowel movement. This vagovagal response may be enough to break the tachycardia and return them to sinus rhythm. If that does not work, you must immediately notify the provider, and assess for causes, document and continue to monitor. The provider will likely order rate control medications like beta blockers or antiarrhythmic drugs like amiodarone.
Symptomatic Ventricular Tachycardia Interventions (Tachycardia, Palpitations, Dropping Blood Pressure, Dizziness, Fainting, Confusion, Syncope, Shortness of Breath Signs of Decreased Cardiac Output): Call a Rapid Response, Prepare to give amiodarone or beta blockers IV.
If the patient does not have a pulse – you will use the defibrillator and follow the ACLS Protocol. Vtach can respond well to defibrillation.
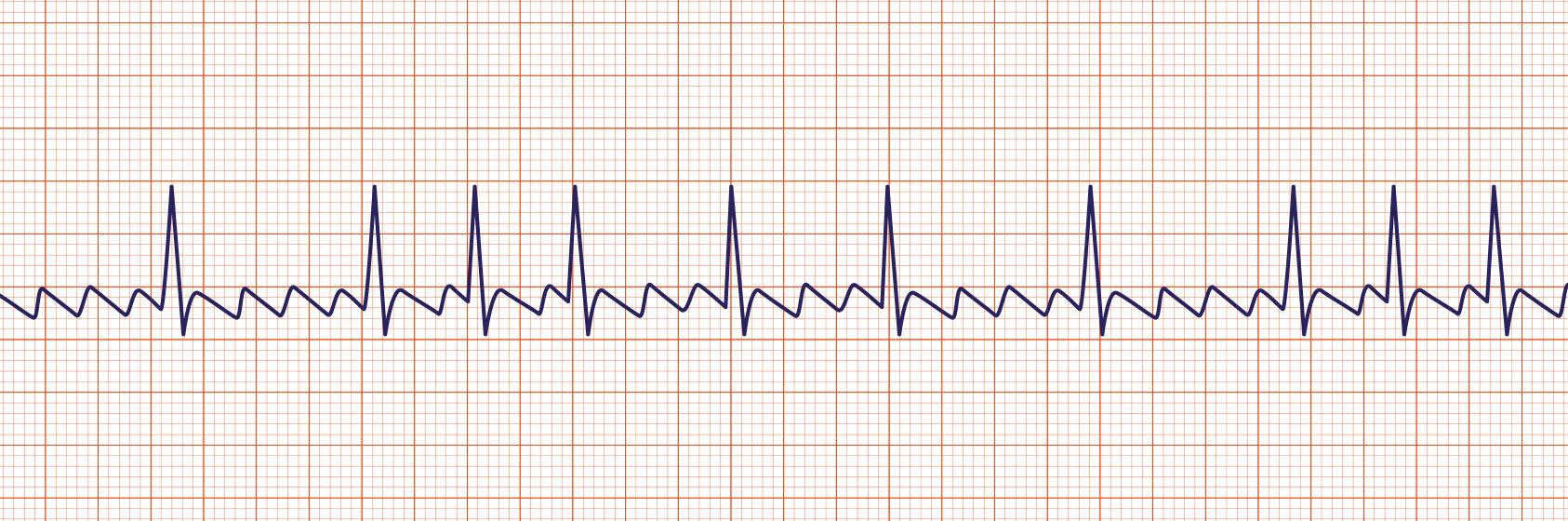
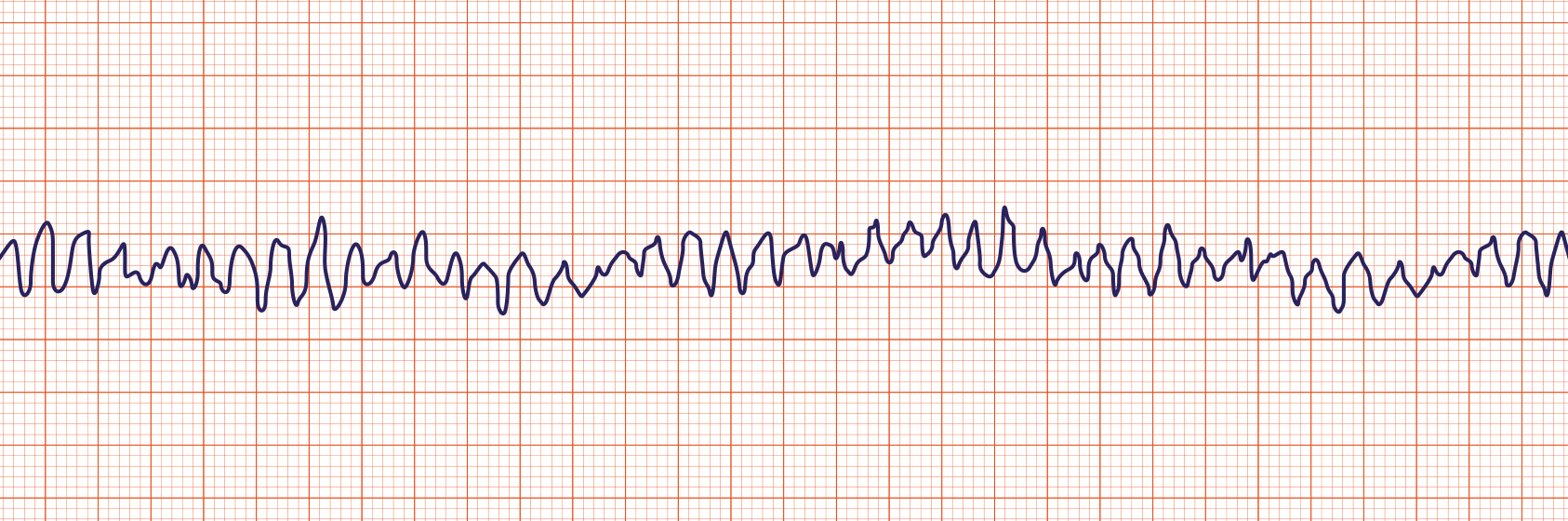
Identifying Ventricular Fibrillation
Ventricular fibrillation (Vfib or VF) is characterized by a ECG that has a chaotic wave pattern and the patient will have no pulse. VF is one of the two “Shockable Rhythms”, which means it may be responsive to electrical defibrillation.
“V-fib means you D-fib!”
This is an EMERGENCY! The first thing you should do is ASSESS YOUR PATIENT to determine if they have a pulse or not. If this is a true rhythm, the patient will NOT have a pulse!
Ventricular Fibrillation Interventions: ASSESS FOR A PULSE! If No Pulse – Call a Code, If your patient is a Full Code, then Begin High-Quality CPR, Defibrillate as Soon as Possible! Follow the ACLS Protocol to Resuscitate your patient.
If your patient does have a pulse, determine if the cardiac monitor leads are correctly attached to the patient. (Sometimes they are hanging on by glue threads or hair and it can cause a similar pattern to show on the monitor).
Identifying Pulseless Electrical Activity
Pulseless Electrical Activity can be virtually any organized ECG rhythm in a patient who is unresponsive and lacks a palpable pulse. This is why frequent rounding on your patients is so essential. Even with a cardiac monitor attached, the only way we can be certain our patients are doing well is if we physically assess them for pulse and breathing.
If your patient does not have a pulse, of if they are not breathing, then you should call a Code Blue and if your patient is a full code, you will follow the BLS and ACLS protocols to resuscitate your patient.
Once you master the technique of measuring and analyzing all of the components of an ECG rhythm strip – identifying which rhythm your patient is experiencing will become so much easier! I hope you find this three part ECG Interpretation for NCLEX series helpful, and I look forward to helping you or someone you know develop strategies for NCLEX Success!
Best Wishes!
-Damion